Opioid addiction isn’t an issue we typically associate with pregnancy, but doctors often prescribe opioids after childbirth to alleviate their patients’ postpartum pain. Regardless of whether you’ve never taken opioids or have overcome an addiction to them, postpartum opioid scripts can lead to serious opioid-related events (SOREs).
But before you understand how these drugs can lead to substance use disorders, it’s essential to understand what they are and why they can be so dangerous.
What Are Opioids?
At their core, opioids are painkillers. They often derive from the opium plant, which possesses natural painkillers that also bring about a sense of euphoria. Morphine is the best-known example of an opioid, and people widely use it to treat pain. As technology progressed, scientists figured out how to make synthetic opioids — that means these drugs mimic the effects of the opium plant, but are entirely human-made. Fentanyl is one of the more common synthetic opioids.
While doctors regularly prescribe opioids as painkillers, there are also illegal, non-prescription opioids. The makers of these drugs tend to dilute them with other, more dangerous drugs to make them more addictive. Street fentanyl, for example, often includes cocaine or heroin, which is another illicit opioid. The result is a more potent drug, giving the user a more intense high.
The potency and dosage are crucial when it comes to opioids, so they are safest when taken on a trained physician’s instructions. Opioids work by sending a signal to the brain, which triggers that feeling of euphoria. But eventually, with continued use, you build a tolerance to opioids and need higher doses to achieve that coveted high. This phenomenon helps make opioids extremely addictive. Even people who take opioids precisely as prescribed can go through opioid withdrawal when their prescription has run out.
The unpleasant withdrawal symptoms, on top of the mental conviction that the body needs opioids, sometimes lead to people seeking these drugs illegally after they’ve completed a prescription. Illegal opioids are often far more potent and seldom pure, making them extremely dangerous.
What Is Opioid Use Disorder?

Opioid use disorder — also known as opioid addiction — is a potential danger when you take any opioids, even prescription ones. Opioid addiction is the chronic use of these drugs, often to the extent that the use negatively interferes in your day-to-day life. It differs from an opioid dependence because dependence is physical, while addiction is both physical and psychological.
Addiction is the physical inability to stop using a drug, resulting in the user finding any way possible to obtain it. The need to get the drug becomes top of mind, prioritized over personal and professional relationships and obligations. The user has only one goal in mind: to seek their drug of use, no matter who or what becomes a casualty along the way. Some common signs that you might have an opioid addiction include:
- Taking opioids more often than prescribed, including “just in case” when not in pain.
- Disturbed sleep patterns.
- Mood swings that go from euphoric to hostile.
- “Doctor shopping” to get a script for opioids, just to have a backup supply.
- “Losing” the medication to get a new prescription.
- Changes in decision-making, especially an increase in dangerous or harmful behavior.
Opioid addiction affects about 2.1 million people in the United States alone, and more than 120,000 people worldwide die each year due to an opioid overdose. Opioid dependence is the physical tolerance of opioids that makes the user feel they need increasingly larger doses to achieve the same high they initially got from the drug. Dependence is part of opioid addiction, but it doesn’t always go hand in hand with addiction. A person taking prescription opioids precisely as prescribed may still develop dependence and could face withdrawal and have the desire to seek more opioids.
Postpartum Opioid Scripts
Doctors often treat postpartum pain with opioids, but a recent study found that people who take opioids for postpartum pain have a higher chance of developing SOREs, such as overdose. The study examined 160,000 pregnant women ranging in age between 18 and 44 who had not taken any opioids in the 180 days before delivery. Deliveries ranged from natural, vaginal births to cesarean sections.
More than half the women in the study who delivered vaginally and a whopping 91% of the women who had a C-section filled at least one opioid prescription for postpartum pain. In addition to that, approximately 10% and 24% of vaginal and C-section births, respectively, filled a second prescription during postpartum. The study found SOREs in more than 4,500 participants, with 69% having persistent opioid use, 19% developing a substance use disorder, 2% having an opioid-related overdose and 0.2% having an opioid-related death.
Opioid scripts after vaginal births are standard, and this study shows the heightened risk this practice puts postpartum people in. But why would doctors prescribe opioids for postpartum pain? The answer has more to do with what sort of pain the opioids are treating, which include:
- Vaginal birth pain, such as uterine cramping and perineal tears
- C-sections
- Breastfeeding, particularly breast engorgement and nipple pain
- General postpartum fatigue
Pain and fatigue are the two most common concerns for postpartum people, since the ordeal of childbirth is mentally, emotionally and physically draining, making both medication and non-medication therapies crucial. Without proper treatment for postpartum pain, people struggle to care for themselves as well as their newborns. Everyone’s pain threshold varies, as does each childbirth event, which means physicians must prescribe a curated postpartum pain management treatment for each patient. It is especially crucial to do so, since one in every 300 opioid-naive patients — meaning they don’t receive opioid-related treatment at all or it’s very rare — are more likely to develop dependence or addiction to opioids after C-section childbirth.
Opioids vs. NSAIDs
Opioids might be some of the best-known painkillers, but they aren’t the only ones available. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are just as useful for treating some types of pain as opioids are — and are far less dangerous and not addictive. However, they can sometimes also be less effective depending on the severity of the pain.
Even after the baby is born, new mothers should consider any medication’s effect on their child. For people who opt to breastfeed, any pain medication used can flow into their breastmilk. Pregnant people who take opioids during pregnancy risk the baby developing something called neonatal abstinence syndrome (NAS), which is when the fetus gets exposed to opioids in the womb, then suffers withdrawal symptoms after birth. In addition to that, the baby can have more health problems as a result, which can endanger its life. These issues are a possibility no matter the dosage of opioids taken during pregnancy. Even if you take prescription opioids exactly as instructed, the opioids are still going to flow through your body and, inevitably, through the fetus’ body as well.
Similarly, taking opioids while breastfeeding can sometimes result in breastmilk with hints of the drug — depending on which opioids specifically, as well as their dosage. Drinking this tainted milk can negatively impact the baby’s respiratory system, make it excessively sedated or even result in the child’s death. NSAIDs, on the other hand, are safer, even if they do leach into the breastmilk the baby feeds on. Medical professionals have deemed medications like ibuprofen safe, even in breastmilk for babies. But, as mentioned, ibuprofen is sometimes not enough to alleviate postpartum pain.
Alternative Options for Pain Management
The American College of Obstetricians and Gynecologists (ACOG), the American College of Nurse-Midwives and the American Academy of Family Physicians established guidelines to effectively and safely help deal with postpartum pain.
Unsurprisingly, these three associations recommend trying nonpharmacological options before taking any medication, and include solutions such as:
- Cold packs for breast engorgement and perineal tears
- Heating pads for uterine cramping
- Breastmilk or breast shield for nipple pain
- Increased frequency of breastfeeding to help with engorgement
If medication becomes necessary, experts recommend trying NSAIDs first, only turning to opioids after the highest dose of NSAIDs has proven ineffective. Since postpartum pain management will vary for everyone, starting with nonpharmacological therapies could be sufficient for some. These over-the-counter drugs can reduce the need to prescribe any medications and, thus, decrease the likelihood of SOREs in the postpartum period.
In the case of opioid prescriptions, the guidelines stress the physician’s responsibility to restrict the number of scripts written, and to inform patients of the correct, safe way to dispose of unused pills.
Chances of Relapse
During pregnancy, chronic opioid use can have severe adverse effects on the fetus, which is why most physicians recommend pregnant people stop using opioids, including prescription ones. Those who taper off opioids amid an active substance use disorder or addiction should do so with professional help for the safest and healthiest results.
However, one study revealed that those recovering from opioid use disorders are at a higher risk of relapsing in the postpartum period. These relapse-related statistics are even more alarming, since many of these people suffered an opioid-related death within the year after their pregnancy ended. Of those deaths, 80% occurred near the end of the postpartum period, after the obstetrician’s final wellness check. The authors of this study hypothesize some reasons for the opioid-related deaths in this population could be a mixture of hormonal changes, postpartum depression, stress and sleep deprivation, plus a reduced tolerance to opioids due to the period of abstinence during pregnancy.
It’s rightfully shed a light on postpartum care, and ACOG has suggested that postnatal care should extend beyond the average six weeks to three months, and should become the fourth trimester of care.
However, the extended time may not be worth anything if a person is unable to afford medical support, such as therapy when the urge to use arises. And with many pregnant people revealing that they got pregnant while under the influence of an opioid and were unable or unwilling to invest in adequate contraception, the likelihood of rehabilitating from an opioid use disorder before trying to get pregnant is unlikely.
Treatment for Opioid Use Disorder
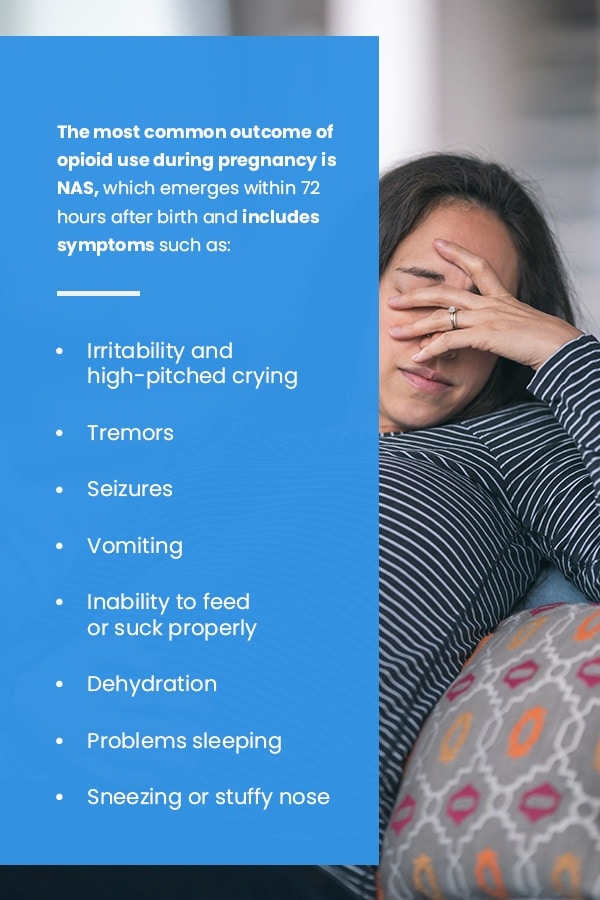
According to the Centers for Disease Control and Prevention, opioid use is prevalent during pregnancy. However, chronic opioid use during pregnancy can result in severe problems for the pregnant person as well as the fetus or the newborn child. The most common outcome of opioid use during pregnancy is NAS, which emerges within 72 hours after birth and includes symptoms such as:
- Irritability and high-pitched crying
- Tremors
- Seizures
- Vomiting
- Inability to feed or suck properly
- Dehydration
- Problems sleeping
- Sneezing or stuffy nose
The severity of these symptoms and which ones the child experiences will vary based on factors such as which opioid the child got exposed to in the womb, which trimester saw the highest exposure and whether the developing fetus may have been subject to other substances in addition to the opioid.
Other potential risks that come with opioid use during pregnancy include:
- Preterm birth
- Longer hospital stay
- Poor fetal growth
- Birth defects
Are you living with an opioid use disorder and are planning to get pregnant? Speaking to a health care provider to come up with a treatment plan for opioid addiction and any co-occurring conditions is the first step to increase your chances of a safe and healthy pregnancy. Because the withdrawal symptoms can be both unpleasant and dangerous, it’s not safe to quit opioids cold turkey. Medication-assisted treatment (MAT) is a good option and can be more effective than supervised tapering off. However, NAS is still a possibility with MAT, thanks to the fact that it combines medication and therapies to overcome opioid use disorder.
MAT is also an acceptable course of treatment for people who are already pregnant and are looking to recover from an opioid use disorder. Methadone and buprenorphine are the two most common medications used in MAT, along with behavioral therapies and medical care. As mentioned, those who have recovered from opioid use disorder during their pregnancy are at a higher risk of relapsing after pregnancy. The additional stressors of being a brand-new parent and having to deal with the hormonal and physical changes that come after childbirth — plus the discomfort and pain, especially after a C-section — can become triggers.
Overcome Opioid Use Disorder With AppleGate Recovery
AppleGate Recovery, dedicated to MAT for opioid addiction, specializes in creating each client’s ideal recovery plan. Using buprenorphine and Suboxone® as well as counseling and recovery services, we tailor our outpatient treatment plans for our clients, based on their individual mental and physical health. We also provide MAT for opioid addiction for pregnant people or those who have experienced a postpartum relapse.
Feel free to walk into our clinic to request a tour of the facility and meet our staff. You can also set up an intake appointment at that time. Our experienced and knowledgeable substance abuse professionals understand the magnitude of getting help for an opioid use disorder and treat all clients with the utmost compassion and discretion.
If you’re ready to take the next step or want to learn more about our services, feel free to get in touch by calling 888-488-5337.


Contact AppleGate Recovery Today
If opioid addiction is impacting your life or the life of someone you care about, reach out to our treatment center. We are here to provide the support and care you need to take the first step toward recovery.
Call 888.488.5337